16 Care Settings to Deploy Remote Patient Monitoring
Explore remote patient monitoring across the continuum of care. No matter the program type, disease state, or care setting, HRS has the experience to deliver results and improve outcomes.
How Does Remote Patient Monitoring Help Patients?
Remote Patient Monitoring (RPM) engages patients in their care to improve clinical outcomes and quality of life. Although RPM has been traditionally been used to assist patients recovering from an acute care episode, the past few years have led to a 1,300% increase in the use of RPM across numerous disease groups and healthcare organizations.
From accountable care organizations (ACOs) to home health agencies to physician groups, healthcare providers across the care continuum are recognizing the value of telehealth technology and RPM programs to deliver quality care services, reduce care costs, and enhance clinical efficiency.

Deliver Better Quality Care for Every Patient, in Every Care Setting
Let’s explore the 16 care settings where remote patient monitoring can best support health systems
and some of the key benefits of RPM for each.
Accountable Care Organizations (ACOs)
ACOs can use RPM to address Medicare penalties for readmissions, financial incentives for chronic disease management, or to involve patients in their own health and encourage them to have an active role in managing their health.
Telehealth can help ACOs reduce unnecessary hospital utilization, improve patient satisfaction, and improve STAR ratings.
Virtual Visits
Increase patient satisfaction and clinician efficiency by offering primary care, specialty care, social work, and more visits virtually.
Data Analytics
Build patient and population-based reports to reduce admissions and provide value-based care.
Bariatrics
Post bariatric surgery, RPM and telehealth can help a patient remain adherent to their dietary guidelines, medication, and exercise regimen, while also providing educational tools on surgical recovery.
Virtual Visits
Host individual and group-based virtual visits to help patients build relationships with their physicians and learn healthy habits from one another.
Biometric Monitoring
Evaluate patients’ progress, identify exacerbations, and hold patients accountable to follow their care plans and meet their goals.
Behavioral Health
With virtual care and symptom surveys, providers are able to track their patients mental health, and intervene if decline is apparent. Through the embedded PHQ9 survey, educational videos, and quizzes, patients are able to improve their health literacy and care plan compliance.
Symptom Surveys
Check in with patients daily and offer regular access to PHQ9 surveys to ensure patients are receiving the care and support they need.
Virtual Visits
Offer both scheduled virtual visits and PRN visits when patients report concerning symptoms or have pressing questions for their providers.
Cardiology and Cardiovascular Services
For patients with cardiac conditions, RPM can help with management of hypertension, medication titration and management, and real-time symptom and vital monitoring (ex. weight monitoring for congestive heart failure and obesity).
Using an array of connected peripheral devices, patients and clinicians can evaluate positive and negative trends in patients’ vital data to mitigate risk of readmission/rehospitalization.
Biometric Monitoring
HRS integrates with biometric monitoring devices that allow clinicians to capture heart, lung sounds, and ECG. Remote monitoring helps reduce care costs and improve outcomes with fewer follow-up visits and hospital admissions.
Data Analytics
Build trends to monitor patients recovery or long term improvement and enable clinicians to quickly recognize exacerbations and prevent adverse outcomes.
Cardiopulmonary Rehab
Telehealth allows providers to offer multidisciplinary (PT, OT, RD) in-home virtual care where they can assess the patient’s biometrics, symptoms, and tolerance to exercise.
Virtual Visits
Enhance the patient experience by providing physical therapy, occupational therapy, and other services virtually, while the patient remains in the comfort of home.
Activity Tracking
Assign patients exercise routines and track their exercise tolerance with activity tracking and customized care plans.
Endocrinology
Leveraging telehealth for glucose monitoring can help diabetic patients manage their symptoms over time. The endocrinologist can, using the data from RPM, make necessary changes to the patient’s care plan that drive beneficial behavior change. Patients can also access a wealth of educational content from one easy to use tablet/smartphone to further their understanding of their condition.
Biometric Monitoring
Consistent monitoring of glucose levels allows clinicians to build trends, monitor progress, and avoid setbacks.
Educational Resources
Help patients develop healthy habits and spur lasting behavior change, improving patients’ long term health and well-being.
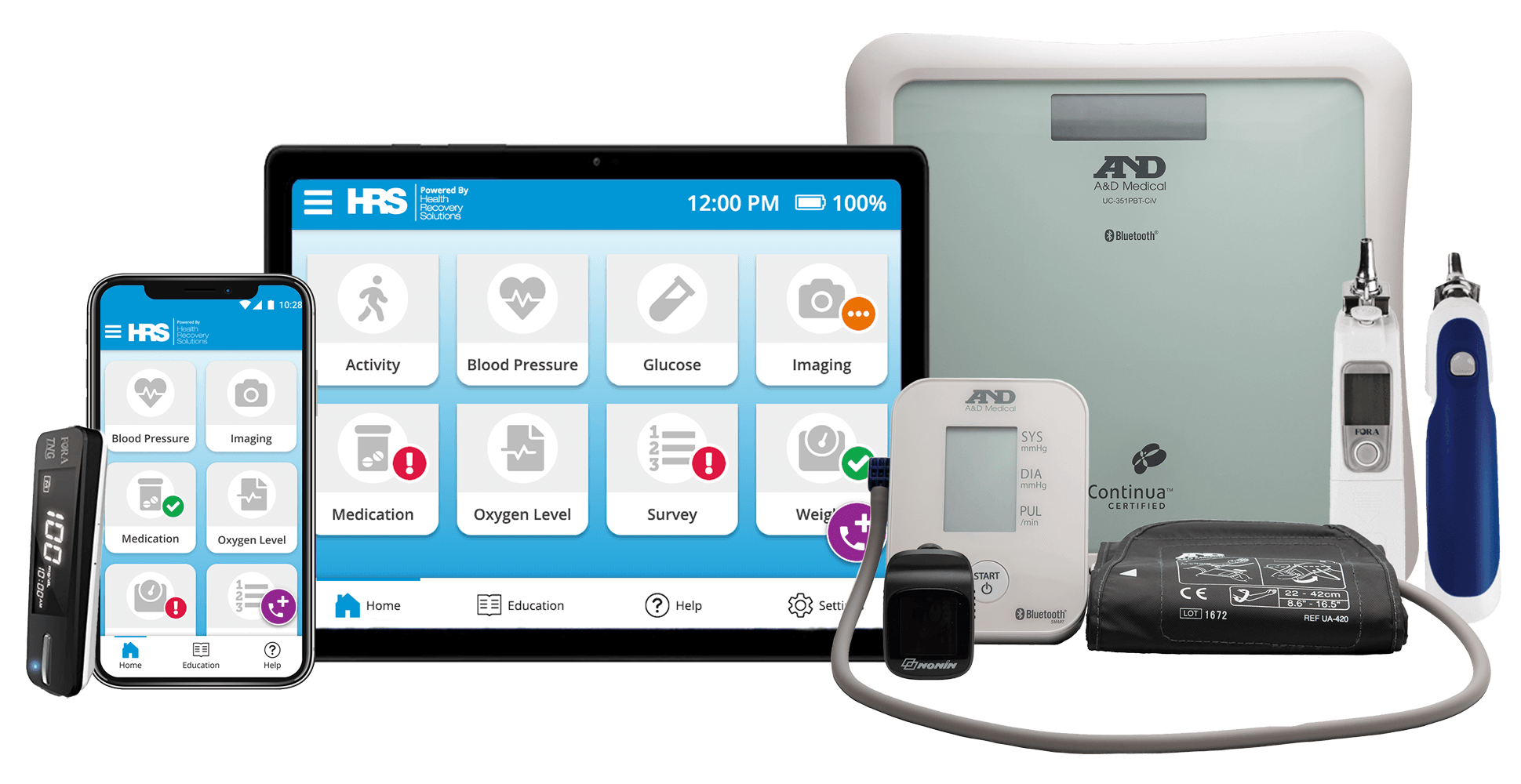
Explore the HRS Suite of Telehealth and RPM Solutions
Super short description about this feature but definitely not lengthy enough for a page. But maybe this one needs to be a little bit longer than the others.
Home Health
Home health providers can offer a continuous care experience with telehealth, one that balances clinical support with self-symptom management. Telehealth helps home health patients avoid readmission by engaging them in their own recovery.
Biometric Monitoring
Track patients’ progress following through their recovery and prevent hospital readmissions by closely monitoring patients’ vitals and symptoms.
Virtual Visits
Provide additional support to patients and reduce care costs by offering virtual skilled nursing, physical therapy, occupational therapy, and social work visits.
Hospice and Palliative Care
For hospice and palliative care patients, telehealth can provide an opportunity for patients to remain in the comfort of home while receiving advanced care and treatment.
Hospice and palliative care patients require specific care planning, educational resources, and the close support of caregivers. Telehealth and RPM enables providers to monitor patients’ symptoms in real-time, such as a patient’s pain, to make adjustments and provide additional comfort.
Educational Resources
A diverse range of educational videos help prepare patients and caregivers for what to expect while receiving palliative or end of life care.
Medication Reminders
For patients in need of complex care plans and detailed medication regimens, providers can leverage medication reminders and tracking.
Hospital at Home
Through hospital at home programs, patients who are eligible for a hospital admission are able to receive hospital care at home. With telehealth and RPM, the provider is able to communicate with and monitor the patient 24/7, ensuring the patient receives high-quality hospital-level care. This results in reduced hospital length of stay, increased bed capacity/throughout and overall a more seamless transition for patients back to their homes.
Biometric Monitoring
The Center for Medicare and Medicaid Services (CMS) requires Hospital at Home programs collect patients vital twice daily. Using RPM solutions allows for more efficient collection of patient vitals.
Virtual Visits
Support the daily evaluation of hospital at home patients, and provide additional support services to patients, such as social work visits.
Everything you need to know about Hospital at Home programs
Explore HRS’ library of Hospital at Home resources to learn how other hospitals and health systems have adopted the model, gain insight into the patient and clinician experience, and review program best practices and supporting research.
How HRS Helps Home Health Agencies with RPM
How HRS Helps Hospice & Palliative Care Providers with RPM
Orthopedics
Telehealth brings post surgical recovery or physical therapy rehabilitation directly into the comfort and convenience of the patient’s home by enabling virtual follow up, virtual physical therapy, and monitoring of orthopedic symptoms.
RPM and telehealth enable surgical teams to engage with the patient remotely through virtual multidisciplinary rounds.
Biometric Monitoring
Ensure patients are recovering post-surgery by tracking their temperature, heart rate,blood pressure, and more.
Symptom Surveys
Check in with patients daily and quickly identify adverse outcomes through custom symptom surveys.
Physician Group
Through telehealth, physicians can remain well connected to their patients, even beyond the office visit. Telehealth helps physicians educate their patients, offers a convenient way to follow up after office visits, and allows for real-time symptom monitoring. Additionally, with the opportunity of reimbursement, physician practices have a strong financial case for converting more of their visits into virtual visits.
Offer the complete advances of telehealth and remote patient monitoring, including symptom surveys, biometric monitoring, and virtual visits, with an affordable, easy-to-use platform.
Medication Reminders
Ensure patients are complying with their care plan and medication regimens between visits by setting medication reminders and checking in through text messaging.
Population Health Services
Incorporating telehealth initiatives into population health initiatives supports the shift to value based care, focusing on holistic patient care and the social determinants of health. With the emergence of “low touch” RPM and telehealth solutions like a BYOD (Bring Your Own Device) option allows for a low cost way to manage large patient populations while still playing an active role in their health and wellness.
PatientConnect Mobile
An affordable solution to deploy telehealth and remote patient monitoring services to an expansive population.
Symptom Surveys
Customize surveys to incorporate questions that provide insight into the social determinants of health patients face.
Prenatal and Postpartum
With telehealth, providers remotely monitor the health of pregnant women, especially those who are rising or high risk. In the prenatal period, where at least 15 face-to-face prenatal visits is the norm, offering telehealth visits improves access and reduces patient burden.
In the postpartum period, providers can use telehealth to monitor for postpartum hypertension, depression, and other conditions, empowering the new parent to remain at home with their newborn.
Biometric Monitoring
For patients at an increased risk of developing preeclampsia, daily blood pressure monitoring provides important clinical insights.
Symptom Surveys
Evaluate patients for preeclampsia, postpartum depression, or other conditions to provide additional support when needed. HRS’ PatientConnect Mobile solution offers an easy-to-use platform for busy moms.
Pulmonology
RPM can help with management of COPD, asthma, and other respiratory conditions, by providing tools for vital sign monitoring, symptom management, and patient-provider communication. Pulmonologists can empower patients to remain adherent to their asthma or COPD care plan with telehealth and RPM.
Virtual Visits
Evaluate potential environmental factors impacting patients’ health and provide educational trainings, including how to use a spirometer or inhaler.
Biometric Monitoring
Advanced monitoring of patients’ vital signs, including heart rate and blood oxygen, helps clinicians to identify and prevent exacerbations.



Telehealth Solutions for Every Patient Population
Remote patient monitoring has traditionally been rooted in post-acute care, but has since expanded into myriad areas of the healthcare system, helping patients monitor their health and stay connected with care providers for every step of their care.
Readmission Prevention
Improve patients’ health literacy through condition-specific educational materials to reduce in-person visits and hospital readmissions
Acute Care Management
Prevent adverse outcomes while allowing patients to recovery in the comfort of home through enhanced biometric and symptom monitoring
Chronic Care Management
Reduce care costs and improve patients’ long term health by educating patients on their conditions, symptoms, and treatments
End of Life Care Management
Support patients and their families through the most difficult period of their life, offering educational resources, as well as counseling and spiritual services.
Related Resources
Our patients have been so committed to establishing a healthier lifestyle through nutritional changes and exercise. They have fought through COVID isolation and have gained so much by being able to meet as a group via telehealth. This would not have been successful without the ability of our patients to collect weights at home and have them download digitally into their chart. The remote monitoring allows us to communicate and encourage our patients as well as collect accurate data.
Telehealth data increases communication with patients. It also increases the communication with the home care team, engages the physician, and produces a result.






![View the Infographic [PDF]](https://no-cache.hubspot.com/cta/default/4064170/497f0431-ca1b-4eb1-9635-8642d5006cc7.png)