Introduction to Remote Patient Monitoring
Across the country, healthcare organizations are embracing remote patient monitoring as a tool to improve patient outcomes and satisfaction, reduce total cost of care, and optimize staffing efficiency.
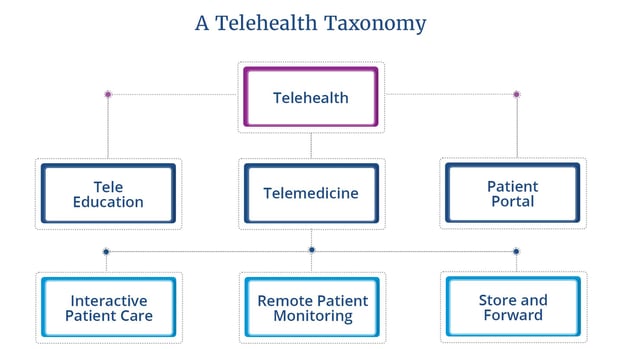
What is Remote Patient Monitoring?
Remote patient monitoring is defined as “periodic, asynchronous, or continuous monitoring and transmission of vital signs, including weight, blood pressure, oxygen saturation, glucose levels, heart rate, or heart rhythm.” Remote patient monitoring falls under the umbrella of telehealth. It is when medical data and health information is collected from an individual in one location and transmitted electronically to a provider in a different location. Simply, remote patient monitoring includes the gathering of patient health data outside of the brick-and-mortar hospital or clinic setting. It allows care to be moved out of the 4 walls of the hospital, into the home setting. Remote patient monitoring is asynchronous, meaning patient information is forwarded (sent), and then stored until the provider has the opportunity to review.
Remote patient monitoring offers many benefits. It provides the clinician with a more accurate picture of their patients’ health—allowing the clinician to see trends in symptoms over time. When clinicians have a more robust data set, they are able to deliver care more proactively and effectively. Remote patient monitoring helps the provider evaluate whether the patient’s condition is stabilized, deteriorating, or improving.
With remote patient monitoring providers are able to access patient data instantly, right at the moment the patient is experiencing pain, confusion, or a symptom exacerbation. When the provider is able to view the full picture of their patient’s condition, they are empowered to deliver more data-driven, proactive care, which in turn, results in improved patient health outcomes and more efficient care delivery. Currently, in the midst of the nursing shortage, RPM eases clinician burden by enabling clinicians to monitor patients from afar.
Remote patient monitoring enables patients to share updates on their vitals from the convenience and comfort of home, allowing the provider to understand in real-time how a patient’s condition is progressing. The patient is empowered to take control and manage their own health, which results in improved patient engagement, increased health literacy, ultimately resulting in improved overall health outcomes and quality of life.
Today, remote patient monitoring is used across a variety of patient populations and care settings and for many conditions, including COPD, CHF, diabetes, hypertension, primary care, post surgical, oncologic care, postpartum and prenatal care, pediatrics, chronic kidney disease ,hospice and palliative care, and more. Remote patient monitoring is one of the most effective ways to manage chronic disease like diabetes, heart failure, COPD, and hypertension, as it enables data-driven proactive care delivery.
How Remote Patient Monitoring Works
Now that you understand what remote patient monitoring is, you’re probably wondering how it works in practice.
How remote patient monitoring works in 5 steps:
- The provider or provider organization decides to deploy remote patient monitoring to monitor their patients. Providers use remote patient monitoring for a variety of conditions to collect a wide range of patient data. Common devices include blood pressure cuffs, pulse oximeters, thermometers, glucometers, weighing scales, ECG/stethoscopes, activity trackers, spirometers, and more.
- With the patient’s consent, the provider deploys remote patient monitoring into the patient’s home (or pocket).
- The patient is provided with the necessary devices to collect their health data, and offered education to help them understand how to use the technology.
- Once the device is set up, at home or work, or even on the go, patients monitor their vitals to collect their health data. Patients can record their vitals once or day, or more frequently, depending on their condition and provider’s direction.
- In real-time, the reading from the biometric device is sent to the patient’s provider, where the provider can then monitor trends and changes. When a reading is out of range, the provider is notified with risk alerts, helping the provider be proactive in their response.
Remote Patient Monitoring Devices and Common Use Cases
The remote patient monitoring devices a patient engages with are unique to each patient and customizable by the clinical team. Devices depend on the patient’s condition as well as their comfort level with technology. Remote patient monitoring devices are non-invasive devices that acquire, transmit, process, and store patient data so providers can understand and track patient symptoms.
There are many remote patient monitoring devices available on the market today, including:
Blood Pressure Cuff
Blood pressure monitoring helps hypertension patients or patients at risk for hypertension keep tabs on and manage their blood pressure over time. Using a blood pressure cuff consistently helps the patient and provider know if medication is working, and alerts the provider of potential health complications as they occur. For postpartum hypertension, at-home blood pressure monitoring can be essential to avoid dangerous complications.

Pulseoximeter
The pulse oximeter can be deployed to monitor the health of any individual with a condition that affects their blood oxygen levels, such as chronic heart or lung issues, COVID-19, or asthma.

Weighing Scale
Example applications include monitoring obese, at-risk patients, and congestive heart failure patients. In CHF patients, weight gain can be an indicator of water retention. When the clinician of a CHF patient sees an out-of-range weight reading, they’re able to prescribe a diuretic, increase a current medication, or call the patient to schedule a visit. For obese patients, or patients at risk of obesity, it’s essential to track weight over time. Obesity is a risk factor for heart disease, stroke, type 2 diabetes, certain forms of cancer, and many other conditions that can often be avoided if proper health is maintained. Tracking weight and keeping it in range helps the patient remain on track and take ownership over their outcomes.
Thermometer
The thermometer can be used for home monitoring across a range of populations, including primary care, pediatrics, and COVID-19. For COVID-19 patients, the thermometer can be used to screen for symptoms, and track patient recovery.

Glucometer
For patients with diabetes, everyday blood sugar monitoring is often essential. Glucometers help patients with diabetes manage their condition effectively, offering many benefits including improved HBA1C and symptom management, increased adherences, and expanded access.

Spirometer
Spirometers, which measure the volume of air inspired and expired by the lung, are helpful tools for patients with respiratory diseases like asthma, COPD, emphysema, and cystic fibrosis.

Wearables like the BioSticker or activity trackers like FitBit or Apple Watch
Wearables can track heart rate, blood pressure, glucose levels, weight gain and loss, and even stress to help clinicians deliver customized, data-driven to patients. Wearables provide a continuous picture of a patient’s health. Examples of wearables include the FitBit, Apple Watch, and BioSticker.

ECG + Stethoscope
An ECG+Stethoscope provides a comprehensive view of cardiovascular function. For patients with conditions affecting their heart or lungs, close monitoring is essential for avoidance of hospitalization or readmission following a hospital discharge.

Benefits of Remote Patient Monitoring for Patients and Clinicians
Patient Benefits
When patients are able to track their health at home, they are more likely to achieve positive health outcomes due to better condition understanding. When a patient is able to self-manage their condition with remote patient monitoring tools, they are likely to reduce costs (both to themselves and the health system), by minimizing emergency room visits, lengthy hospital stays, and preventing readmissions.
The top 13 benefits of remote patient monitoring:
- Improved data driven clinical decision making
- Helps patient improve self management and care plan adherence
- Cost of care reduction for payers and providers
- Boosts net patient revenue
- Reduces patient’s expenses and improved work productivity
- Improves access to care
- Builds patient engagement
- Optimizes clinical staff efficiency and combats clinical staff shortages
- Prevents the spread of infectious diseases and Hospital-Acquired Infections
- Improves patient experience and satisfaction
- Expands referral opportunities and improves retention
- Improves the clinician-patient relationship
Remote Patient Monitoring Reimbursement and Billing
Providers can bill for remote patient monitoring with 5 primary CPT codes. The codes provide a financial structure for qualified providers to bill for the time spent, services rendered, and equipment used. The Centers for Medicare and Medicaid services outlined remote patient monitoring in their final ruling on the 2021 Medicare Physician Fee Schedule.
RPM Billing
-
99091: can be billed $59 once per 30-day period for a minimum of 30 minutes of review data only by physicians or qualified health care professionals
-
99453: covers the set up and patient education on remote patient monitoring equipment including initial setup of devices, training and education, and any services needed to enroll the patient on-site ($21)
-
99454: covers remote monitoring of physiological data with a device; reimbursement of $69 can be filed once every 30 days
-
99457: provides a $54 reimbursement each calendar month for a minimum of 20 minutes of live communication with the patients by physicians, qualified health care professions or clinical staff
-
99458: is an add-on for CPT code 99457 and cannot be billed as a standalone code; it is used for each additional 20 minutes of remote monitoring (allows for $43 in billing per calendar month)
Choosing a Remote Patient Monitoring Vendor
When choosing a remote patient monitoring vendor, it’s essential to ask the right questions. Start with determining what the goal of the remote patient monitoring program is, from there, determine what features and functionality are necessary for your program to be successful.
Feature functionality and Bluetooth devices
Previous successes and case studies
Product roadmap and strategy
The clinician and patient experience
Clinical monitoring
Implementation process
Technology connectivity (cellular and wifi)
It is especially important to focus on the services beyond the product itself. For the remote patient monitoring program to be successful, support services are crucial. Consider questions like “what does implementation look like for both the patient and provider organization?” “Who from the vendor supports the program after implementation?” “Does the vendor offer support with clinical workflows and reimbursement strategies?” “If the patient or clinician has an issue with the product, who do they call for support?”
Building and sustaining a successful telehealth program includes many components and moving parts. To ensure lasting success, it is imperative that the vendor is able to offer operational support and guidance throughout the tenure of the program.

The People Behind HRS Products
Behind HRS’ award-winning products are support teams across HRS that give clients the strategic, clinical, operational, and technical support they are looking for to drive long-term, positive outcomes for the organization.
Setting up your Remote Patient Monitoring Program
There’s a lot to consider when setting up a new telehealth program. Start with determining your goals for the program—what are you hoping to achieve with remote patient monitoring? Think specifically about both patient metrics and staffing ones. From there, think about the patient populations you’re looking to serve, who will staff the telehealth program, and how you’ll establish clinician and patient buy-in.
Today, remote patient monitoring is used across a range of healthcare organizations for a diverse group of patient populations. With it, patients are improving outcomes, while healthcare organizations are improving efficiencies and reducing cost of care.
Download the 6 Essential Steps to Building a Scalable and Profitable Telehealth Program White Paper
In this white paper, learn about:
- Establishing goals
- Determining your financial plan
- Choosing a technology partner
- Building clinician and patient buy-in
- Other essential factors to consider to ensure your program is successful
