Growing at a rapid pace in 2020, telehealth has quickly expanded to serve a range of patient populations. For cardiovascular patients especially, telehealth can be used to manage symptoms, improve patient engagement, and ensure continuous connection between the patient and their clinician(s).
Now that the initial wave of COVID-19 infections has passed, health systems are expecting a continuing surge in appointments for patients with cardiovascular conditions. Because of COVID-19, treatments were delayed, and appointments cancelled. Patients were not receiving their usual cardiological care.
Many health systems across the country adopted telehealth early on to help manage these patients; others have yet to do so. To stay ahead of exacerbations and life-altering symptoms healthcare providers need to make a shift toward wide adoption of telehealth and RPM to ensure their patients receive quality care at home. For cardiology patients, telecardiology, i.e. cardiology focused telehealth care, could be the answer.
 Source: Keck Medicine of USC
Source: Keck Medicine of USC
How Patients with Heart Conditions Benefit from Telehealth
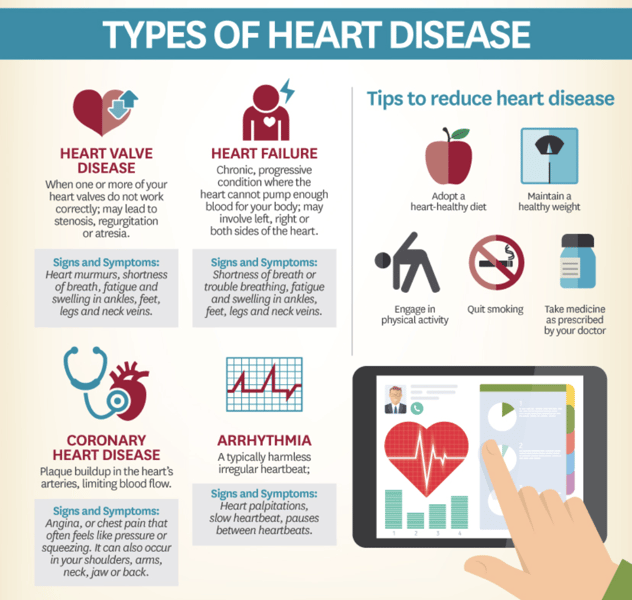
Spanning all ages, from pediatric to geriatric patients, individuals with heart conditions such as hyperlipidemia, syncope, acute cardiovascular disease (CVD), congestive heart failure, cardiac arrest, and arrhythmia, are seeing the benefits of telecardiology now more than ever. It helps to remove the barrier of transportation to and from appointments or rehabilitation, while also increasing patient engagement.
With video and voice calling clinicians can in real-time monitor heart rhythm, breathing patterns, blood pressure, edema, and more. They can make necessary adjustments to a patient’s medication, exercise or diet routine and encourage control and confidence in their health. Catching symptoms or vital changes early can help avoid exacerbations and save a life.
Overcoming Challenges with Cardiology Patients
While widely used across the country, telehealth and telecardiology is especially beneficial for patients in rural areas who are hours away from their nearest clinician. As rural area health systems continue to experience closures, some clinicians have partnered with larger systems and hospitals to treat patients. This allows patients to remain in their nearest hospital instead of traveling hours away. Integrated health systems with doctors and hospital teams are coming together to offer patients the cardiology care they need at home.
Figure 1. Applications, advantages, considerations for implementation and current challenges of telehealth in cardiovascular disease prevention. Source: American College of Cardiology
Reimbursement challenges continue to present themselves throughout the healthcare system. Changes in healthcare regulations and reimbursement have greatly impacted telehealth during the COVID-19 pandemic. The Centers of Medicare and Medicaid Services (CMS) and many larger payers have expanded reimbursement for telehealth. For example, according to American College of Cardiology, telephone only visits, which have previously not been covered, are now reimbursable during the public health emergency. Clinicians can now offer a wider range of services without worrying about reimbursement costs or the cost to patients.
Paving the Way
Telehealth utilization continues to grow across the country as telehealth programs become more widely available, and as providers start to realize both the efficacy of the service, but also their patients’ desire to receive care at home. For cardiology patients especially, telehealth is an important tool. It helps them manage their condition from home and avoid the requirement of traveling to the clinic for an in-person visit. Keeping on top of vitals and abreast of symptom changes is essential for cardiac patients - telehealth helps them achieve these goals and ultimately avoid symptom exacerbations and unnecessary ED visits.