“What do you think about this Coronavirus? Should we be worried?” The question was posed to me in early February by the CEO of Health Recovery Solutions (HRS), Jarrett Bauer. For me, as the VP of Clinical Services, it was a natural call. I should know. I was certain it was no big deal. That’s what we were being told. And we had the best health care system in the world. And the CDC was the world’s most trusted expert in infectious disease. Surely there was nothing to worry about. But the rumblings were there, and the cases were growing. Within a few short weeks, we were in the midst of the worst worldwide pandemic in our lifetime. New York City became the terrifying reality of what a pandemic could do to an unprepared nation. As the lockdowns expanded, we sat in shocked silence at the task force daily news briefings waiting for Dr. Fauci to reassure us in some small way. Any kind of way.
The HRS office was forced to close, but the real work had just begun. People were being asked to quarantine at home, watch for symptoms and only come to the hospital if they had trouble breathing. HRS, recognizing that home health already cared for an at-risk population, the elderly with complex chronic conditions, understood that virtual care was going to be critical. Health Systems too, faced with bed shortages, understood they would have to send patients with non-life-threatening conditions home. PPE for home health staff was limited, patients were refusing visits. Overnight, agencies had to go virtual. HRS responded quickly, mobilizing resources to meet the increased demand for remote care.
Leadership did what good leaders do, offering direction, support and focus on the mission - take care of patients. The Sales Team connected with clients to assess their needs and facilitate scaling up. The Client Success Team brainstormed with clients to address the growing need and seek creative solutions. Marketing kept the communication lines open providing real time information and resources for clients and the team. HR kept spirits high. Data Scientists identified client, patient and system trends. Developers embedded the new COVID content on the platform. Technical Support fielded patient and team questions. Logistics worked day and night to meet the new demand. The warehouse expanded. Finance made it happen. It wasn't always pretty. It wasn't perfect. But everyone was all in. The effort was monumental.
My role was to develop tools and interventions to address the care for at risk and COVID positive patients. The Virtual Visit Guide was released to help nurses, physical and occupational therapists and social workers through the process of effective virtual care. Many, if not most, were new to connecting with patients remotely. Virtual care exploded. From the first to second quarter of 2020, virtual visits grew from 9K to 24K. Necessity ignited a culture shift in a manner of weeks. Virtual care was now an established and valued practice.
The COVID Care Plan was released soon after. Designed to help patients and their caregivers identify the symptoms of COVID, the Care Plan is delivered directly to the patient’s tablet or the mobile application. The COVID Zone Tool asks the patient to identify the Green, Yellow or Red Zone based on their symptoms. This easy to use self assessment tool not only teaches the patient to be vigilant in self-reporting, it also gives the clinician clear information about the patient' s status. Daily Symptom Surveys, revised to include new symptoms as they were identified, now include the loss of taste and smell. Biometric measures include temperature and pulse oxygenation, 2 critical measures of the virus. The identified symptoms and the progression of the virus seemed to change daily. As new or conflicting information emerged, we did our research to ensure the information and tools we shared were the most accurate and up to date. The PHQ9 Depression Screening was added to the Care Plan to identify those suffering due to the increased isolation, anxiety and worry. Thousands of patients have used the COVID Care Plan, both at risk patients and COVID positive.
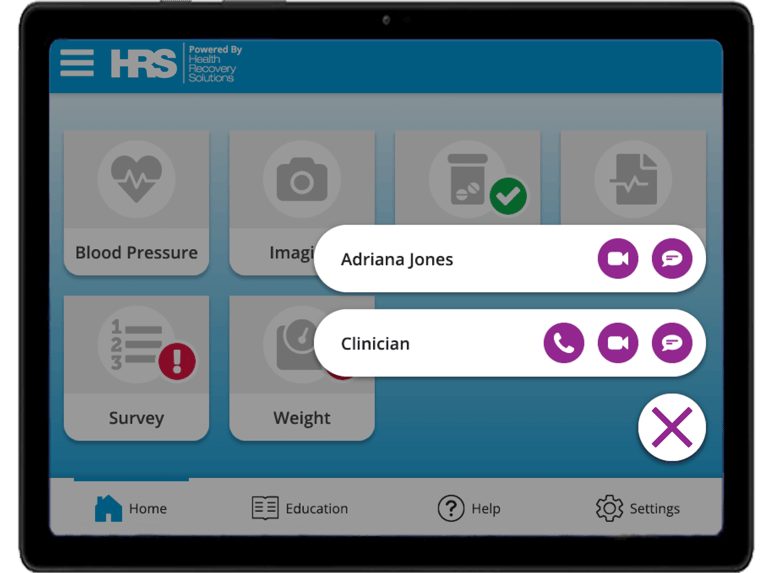 Depression Screening Symptom Survey Question on the Mobile Application, Communication Tools on the Tablet
Depression Screening Symptom Survey Question on the Mobile Application, Communication Tools on the Tablet
Today, we are all changed in some way from the experience. The loss is incalculable. As of the date of this blog, 128,000 people have died in the US. Over 300 health care workers have died. Many believe those numbers are much higher. And the grim reality is there are many more deaths to come. The surge has now intensified across the South and West. The CDC warns that this is only the beginning. The WHO predicts that worldwide, the worst is yet to come, a dim and discouraging forecast as the hopes for warm weather to dampen the virus evaporate. Testing challenges persist as long lines of cars snake toward testing sites in the newest hot spots. Tests results can take a week or more making contact tracing impossible. States are rolling back their openings. Mask wearing, such a simple thing, is not the norm. Images of crowded beaches with the 4th of July approaching and the ongoing protests increasing potential risk are unsettling. Quarantine fatigue is a real thing, and burn out for our courageous health care workers is even more real and more threatening.
But those of us in healthcare are an optimistic lot, and hope outweighs fear. Antibody testing is expanding. Promising and proven drugs are emerging. A vaccine will be effective, and it will be available in record time. Hospitals have a game plan for increasing ICU beds. And practitioners have a better understanding of treating those afflicted.
So much has been done, so much has been learned, but these are still unsettled times. Many of us now appreciate the smaller things, to not be so busy, to take time for ourselves, to connect more with friends and family. Our future is too uncertain not to. But for HRS, and all of us who support the care of patients, the work and the hope continues.