The United States has the highest maternal mortality rate in the developed world and is one of only two developed countries where this number is steadily rising, the other country being Serbia. Across the globe and in particular over the last 30 years, there have been remarkable improvements in maternal and reproductive health. So, what’s the story? Why is the US’ maternal mortality rate among the highest and increasing, and what can be done by providers and patients to reduce the risk of dangerous complications?
Postpartum Hypertension in the United States
Over 700 women die from complications related to pregnancy in the United States each year. Of these 700 deaths, over 460 (around 2/3rds) are preventable. 50,000 women suffer from life threatening complications of pregnancy each year, many of which are caused by chronic conditions such as high blood pressure, diabetes, heart disease, and obesity. There are other important statistics to consider when seeking to understand why the US has the highest maternal mortality rate of any developed country, including:
-
Significant racial disparities (the most notable disparity in mortality rates in the United States) – black women are three to four times more likely to die in childbirth than white women (regardless of education, income, or other socio-economic factors).
-
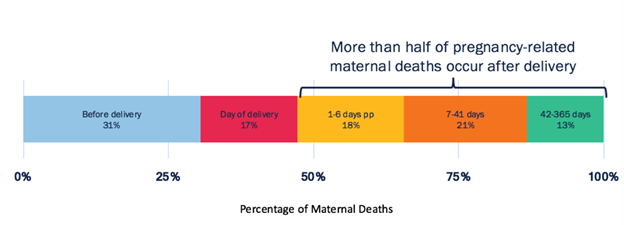
Of the 2,900 pregnancy related deaths between 2011 and 2015 (for which timing was known), 31% took place during pregnancy, 36% occurred during or in the week after delivery, and 33% happened between one week to one year postpartum.
-
The leading cause of death during delivery was obstetric emergencies such as hemorrhaging and amniotic fluid embolism. In the week following childbirth, high blood pressure, severe bleeding, and infection caused most deaths. Beyond the immediate postpartum period, cardiomyopathy and weakened heart muscles were the most common causes.
-
These numbers are staggering and often largely avoidable. One consistent cause of complications and even death in postpartum mothers is postpartum hypertension. In the United States, 10% of pregnancies are affected by hypertension-related disorders. The most common cause of postpartum hypertension is high blood pressure from gestational hypertension or pre-eclampsia that persists after delivery. High blood pressure can also be caused by previous chronic hypertension or eclampsia. This is a condition that can be controlled with close and careful monitoring.
Blood Pressure Home Monitoring for the Postpartum Patient
So important in the postpartum period is close monitoring of signs and symptoms of hypertension and preeclampsia. Through careful monitoring, dangerous complications such as hypertensive encephalopathy, liver hemorrhage, renal failure, the development of eclampsia, ischemic stroke/cerebral hemorrhage, pulmonary edema, and cardiomyopathy can be avoided.
Blood pressure home monitoring is just one way providers can monitor their postpartum patients for dangerous symptoms. As mentioned previously, women at the highest risk for postpartum hypertension are those who had previous chronic conditions, pre-eclampsia, or hypertension during pregnancy. Upon discharge, postpartum mothers can be sent home with a telehealth solution where they can monitor their vitals, communicate with their provider, and engage in education about risk factors and other important elements to be aware of during the postpartum period.
When armed with telehealth solutions providers can rapidly detect concerning signs and symptoms in postpartum women and intervene before the situation becomes critical.
Source: Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130(2):366-73.
Access to Care in the Postpartum Period - Reducing the Barrier with Telehealth
Arguably, the most notable disparity in the mortality rates in the United States is due to race. The maternal mortality for black women is 42 per 100,000 live births, while it is 12 per 100,000 among white women. There are many factors that likely contribute to this disparity, one of which is the fact that black women have poorer access to high quality reproductive health information and services than white women. Women living in underserved communities and in certain states with strained health systems, inaccessible care, high rates of poverty, or other circumstances, experience significantly higher maternal mortality rates than the national average.
Telehealth is one solution to improve the access barrier that many women experience. By providing tools for education and biometric monitoring, postpartum mothers can receive quality health care regardless of location. Many women do not receive paid parental leave and/or sick leave, or are unable to get to appointments due to transportation or childcare needs. Telehealth ensures that patients still receive the quality care they need, even if they cannot get to the hospital or clinic.
Postpartum Hypertension & Telehealth Supported by the Literature
In recent years, research has largely supported the use of telehealth for monitoring postpartum hypertension (PP HTN).
A recent non-randomized control trial between March 2016 and July 2017 of 214 intervention and 214 control participants found that telehealth with remote monitoring allowed for earlier detection and significant reduction of hospital readmission among postpartum patients with hypertension. The intervention group received a tablet device and Bluetooth equipment including a blood pressure cuff, pulse oximeter, and weighing scale. Controls received standard outpatient care directed by the American College of Obstetrics & Gynecology (ACOG).
Among telehealth participants, 130 (63%) experienced an increase in PP HTN requiring treatment and 62 (30%) developed severe HTN after discharge. There was a significant decrease in HTN related readmission in the telehealth group (.5%) vs control (3.7) group.
Another study out of the University of Wisconsin found that telehealth identified hypertension complications prior to the recommended follow up time, and that participants preferred home monitoring over clinic monitoring. This single cohort feasibility study consisting of 55 participants, evaluated postpartum telehealth intervention for blood pressure management after discharge. Among the study participants, 53% required treatment due to exacerbations in blood pressure after discharge, in which 16% were severe. There were no hospital readmissions during the study period.
As of April 2018, there are new guidelines for postpartum care from the ACOG that redefine the postpartum visit. These new guidelines replace the one-off six-week postpartum visit with 12 weeks of ongoing support, tailored to the needs of each individual woman. For patients who prefer to receive care at home, require continual monitoring, or live in rural or underserved areas, telehealth is a great option to ensure the guidelines outlined by the ACOG are followed.
Meeting the Postpartum Patient Where She is With Telehealth
It’s important to consider that in many cases, the postpartum patient has a new baby at home. She’s focused on caring for an infant while also dealing with her own needs, both physical and emotional. In many cases, postpartum mothers are also effected by the “baby blues” (75% of all new mothers) or postpartum depression (1 in 10 mothers). With monitoring at home, providers and the US healthcare system in general can meet these patients where they are, in the comfort of their own homes, while still monitoring symptoms and ensuring interventions occur before crises arise.
References:
Addario, L. (2018, December 13). Can the lives of mothers giving birth be saved? Retrieved from https://www.nationalgeographic.com/culture/2018/12/maternal-mortality-usa-health-motherhood/#close.
Creanga AA, Syverson C, Seed K, Callaghan WM. Pregnancy-related mortality in the United States, 2011-2013. Obstet Gynecol. 2017;130(2):366-73.
Hoppe, K. K., Thomas, N., Fedenia, K., Zernick, M., Zella, J. B., Shah, D. M., … Johnson, H. (2019). 451: A non-randomized controlled study: Telehealth with remote patient monitoring vs standard care for postpartum hypertension. American Journal of Obstetrics and Gynecology, 220(1). doi: 10.1016/j.ajog.2018.11.472
Hoppe, K. K., Williams, M., Thomas, N., Zella, J. B., Drewry, A., Kim, K., … Johnson, H. M. (2019). Telehealth with remote blood pressure monitoring for postpartum hypertension: A prospective single-cohort feasibility study. Pregnancy Hypertension, 15, 171–176. doi: 10.1016/j.preghy.2018.12.007
Optimizing postpartum care. ACOG Committee Opinion No. 736. American College of Obstetricians and Gynecologists. Obstet Gynecol 2018;131:e140–50.
Pregnancy-related Deaths. (2019, May 7). Retrieved from https://www.cdc.gov/vitalsigns/maternal-deaths/index.html.
