The Home Health Value Based Purchasing Model (HHVBPM) was piloted in 9 states in 2016. Based on the success of the model, CMS expanded it nationwide in 2022. The pilot realized a decrease in emergency room visits and hospitalizations, improved patient mobility, and reduced Medicare spending.
The Timeline
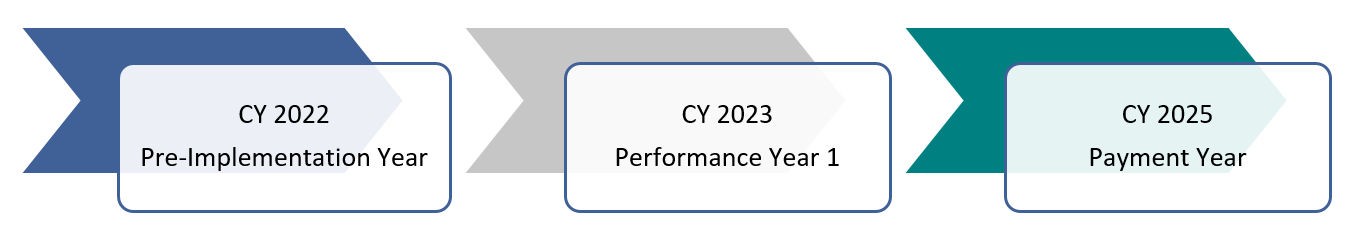
2022 is the baseline or Pre-implementation Year.
2023, the Performance Year, is compared to 2022 to determine the Total Performance Score (TPS Score), which translates into the Adjusted Payment Percentage (APP).
Calendar Year 2025 is the first payment year where the APP from –5% to 5% will be applied to all Medicare fee-for-service payments.
That can be a significant gain or loss and requires a strategy that maximizes the potential gain.
With additional Medicare cuts looming, capitalizing on the HHVBPM is critical.
More than likely, you are already well on your way since the year is moving quickly. But now may be a good time to reset. Are you on the right track or not? If you are not making progress, it is time to rethink your strategy.
First, let’s look at the measures that are included.
Targeted Measures
The selected OASIS (Outcome and Assessment Information Set) outcomes including the composite measures of Self-Care and Mobility, Oral Medications, Dyspnea and Discharged to the Community count 35% of the total.
Acute Care Hospitalization (ACH) and ED (Emergency Departments) Utilization, from claims- based data, counts for 35% of the total score, but it’s important to note that ACH alone is worth 26.25%, by far the largest single factor in determining your score. And lastly, the HHCAHPS Score counts as 30% of the overall score
Home Health Agencies receive points based either on their achievement level relative to baseline threshold values or improvement relative to their baseline performance.
It is critical that you have a plan for each of the individual metrics, including understanding where you are now. How are you trending: up or down, and why? Once you understand the why, you can develop your action plan.
Acute Care Hospitalization
For example, if your Acute Care Hospitalization rate is higher than the Strategic Healthcare Programs (SHP) state and/or national benchmarks, it is time to get busy.
To get to the why of your hospitalization rate, hospitalization record review is critical. Fortunately, SHP can help you. Review the hospitalization rates by clinician. Who has the highest rates and who has the lowest? What do they do differently?
Highlight examples of success stories - ED or hospitalization avoidance. Let your staff tell their stories of success. Hearing from their own peers can often be very compelling for your clinical staff. Lead a discussion around high-risk patients and how to identify red flags before they lead to a poor outcome. Clinicians can learn so much from a hospitalization review, but it should be done in a teachable way and not in a punitive way. Allow clinicians a safe place to speak freely about their challenges. The key is not to make assumptions about your hospitalization rates, but to really understand what is driving it.
Continuity and Coordination
Two of the most significant impacts on outcomes, including hospitalization, are continuity and coordination of care. If you are short-staffed (and who isn’t?) chances are patient visits are frequently being handed off, delayed, or even missed. The value of a nurse case manager who truly follows their own patients throughout the episode of care cannot be overestimated. High-risk patients especially require continuity and coordination among the disciplines. If you can only do one thing, get that piece right.
Improved continuity and coordination can be achieved by creating small multidisciplinary teams or PODS. The patient is assigned to the POD, and no one outside of the POD can see the patient. That limits the number of nurses and other disciplines that see the patient and encourages better care coordination. The POD becomes the expert care team for a defined patient population. Develop POD communication tools to make it easy for the team to communicate quickly and effectively. Agencies that truly tap into the whole care team achieve better outcomes, and teamwork improves staff morale.
Patient Teaching
What and how we teach patients is an often-overlooked strategy. Not all patients learn the same way, and not all clinicians are excellent teachers. We often give patients more information than they can absorb. They are often sick and recovering from a hospital stay. They come home with stacks of information they will never read.
Keep it simple and to the point. What does the patient need to know? They need to know when and why to take their medications, and they need to know the signs and symptoms related to their illness that matter. Zone Tools or Stoplight Tools are ideal teaching and self-management tools. Use them consistently across all teams and disciplines. Asking the patient what Zone they are in provides a teach-back opportunity and reinforces self-management skills for the patient. It also informs the clinician of the patient’s perceived symptoms and issues that may need to be addressed.
These are just a few of the strategies that should be hardwired into your process. Managing your hospitalization rate is just one driver of the model, and while it carries the most weight, that alone cannot get you the maximum score. However, the strategies outlined here form the basis for improving all your quality measures because they are at the core of a patient-centered model of care.