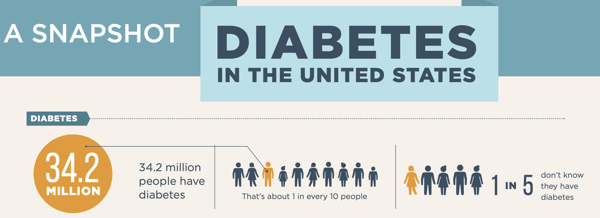
According to the CDC, 10.5% of the US population (approximately 34.2 million people) lives with diabetes, making it one of the most prevalent chronic diseases in our country. Many individuals with diabetes have sub-optimal control of their disease due to poor adherence to their treatment plan, noncompliance with doctor’s visits, or a general lack of understanding about their condition. To properly manage their condition, diabetic patients require an effective and individualized chronic care management plan that focuses on the areas mentioned above - making this patient population a great candidate for telehealth.
Source: Centers for Disease Control and Prevention. National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, US Dept. of Health and Human Services; 2020.
There is a steep economic toll for diabetes on both patients and the healthcare system. For people with diabetes, medical costs are more than twice as high as those without diabetes. In 2017, the total cost of diagnosed diabetes was $327 billion in the US. Telehealth can help curb these figures by optimizing clinical efficiency, reducing office visits and their associated costs, decreasing costs associated with transportation, reducing costs associated with disease exacerbation (due to improved outcomes), and decreasing readmission and unnecessary healthcare facility utilization.
One study out of University of California at Berkelely found that digital health tools can help reduce a patients' monthly healthcare costs by 22% while also improving long-term health outcomes and practice efficiency.
Like other chronic diseases such as CHF, COPD, and hypertension, telehealth can serve as a valuable tool for both diabetic patients and their providers. Incorporating telehealth and RPM into diabetes care management can improve HbA1c and comorbidities, improve patient self-management skills, enhance positive behavior change, expand access to care, and increase patient adherence. Advantages to incorporating telehealth and RPM into diabetes care management include:
1. Improved HbA1c
Providers who incorporate telehealth and RPM are able to track and trend a patient's blood sugar and make more timely interventions to address any variances. The HbA1c is the most accurate indicator of the patient's compliance with their treatment plan and goals. The American Diabetes Association recommends targeting a fasting blood sugar (BS) of 130 or less and a post prandial BS no greater than 180. Closely monitoring and managing those parameters can achieve a HbA1c of 7 or less, or an average BS over the last 3 months of about 150, the recommended goal.
Many diabetics suffer significant comorbidities that can affect their overall health and seriously impact their diabetes. Hypertension is common among diabetics - 73.6% of individuals aged 18 years or more with diabetes, have hypertension. Through RPM, providers are able to monitor their patient’s blood pressure in real time, ensuring that they are able to effectively manage their patient’s symptoms and condition.
Another common comorbidity of diabetes is depression. Individuals with diabetes are 2-3x more likely to suffer from depression than those without diabetes. Depression, in addition to the many factors listed above, can be managed and monitored virtually through telehealth.
2. Improved Patient Self-Management
Successful patient self-management and patient engagement is critical to managing chronic disease and telehealth is a powerful self-management tool. Disease specific video education (medication and nutritional education) and teach-back quizzes, as well as smoking cessation programs and other educational resources are effective tools to engage patients in developing their self-management skills.
Following an individualized meal plan, getting physical activity, avoiding tobacco use, adhering to medications, and regularly monitoring blood sugar are essential factors to prevent diabetes complications. Telehealth helps patients retain and maintain these behaviors by providing nutrition and smoking cessation education, enabling activity tracking through wearables, and facilitating virtual consults with specialists and sessions with coaches and dietitians. When individuals understand why and how they need to change their behavior, they are more likely to do so. Telehealth first helps build this understanding then helps the patient maintain the necessary habits.
3. Expanded Access to Providers
Access to diabetes care varies widely across the country and is influenced by many factors, such as geographic, economic, and social conditions. Telehealth helps bridge the gap of care and improve access. Especially in rural areas, where patients may not have access to specialists, care can be reached through telehealth. Additionally, telehealth can be used as a prevention tool for at-risk patients (an estimated 88 million Americans over 18 have pre-diabetes). The CDC is working to prevent at-risk individuals from developing type 2 diabetes through the National Diabetes Prevention Programs (DPP). Telehealth can help clinicians deliver this program in areas they otherwise would not be able to access, ensuring that patients in rural areas can access education and other preventative measures at the same rate as their suburban or urban counterparts.
4. Increased Adherence
Adherence is a critical component of diabetes care management. When a patient adheres to their care plan, they are more likely to see positive results and avoid disease complications. The patient must be in the driver’s seat to effectively manage their condition but telehealth helps ensure they are comfortable behind the wheel.
A recent randomized controlled trial found that telehealth can improve patient adherence among patients with type 2 diabetes. Telehealth improved adherence by allowing patients to report their daily blood glucose readings easily and facilitated regular communication between the patients and the nurse case manager. Additionally, the telehealth program enabled nurses to respond quickly to a patient’s status and titrate medications when necessary.
Telehealth and Diabetes Care Management
Incorporating telehealth into diabetes care management can lead to increased access to care, improved adherence, better managed symptoms, and can also facilitate lifestyle modifications and behavior change. Additionally, telehealth can enhance clinical efficiency, clinical decision making, and patient-self management skills, while reducing costs to the healthcare system.
For a patient population whose outcomes so clearly rely on self-management and clinician communication and engagement, telehealth is certainly a no-brainer.
